By Jenny Perez
Supporting your patients physically and emotionally is paramount in managing their overall health, especially reproductive well-being. In this guide, we explore seven potential factors/signs of infertility, including often-overlooked environmental factors that may be passively contributing to reproductive health challenges, and how you can monitor and provide guidance for their health management.
Understanding the Complexity of Infertility
Navigating life's journey while also trying to manage the challenges of trying to conceive can be extremely challenging for your patients. Infertility is a condition of a person's reproductive system, causing a woman not to be able to get pregnant after one year of trying to conceive.1
According to the World Health Organization (WHO), that translates to approximately 17.5% of the adult population worldwide, or about 1 in 6 adults.2
Here in the United States, the Centers for Disease Control and Prevention shares that about 10% of women (6.1 million) in the United States who are of childbearing age (ages 15-44) have difficulty becoming pregnant or carrying out a pregnancy to term.3
Infertility is Not Gender-Specific
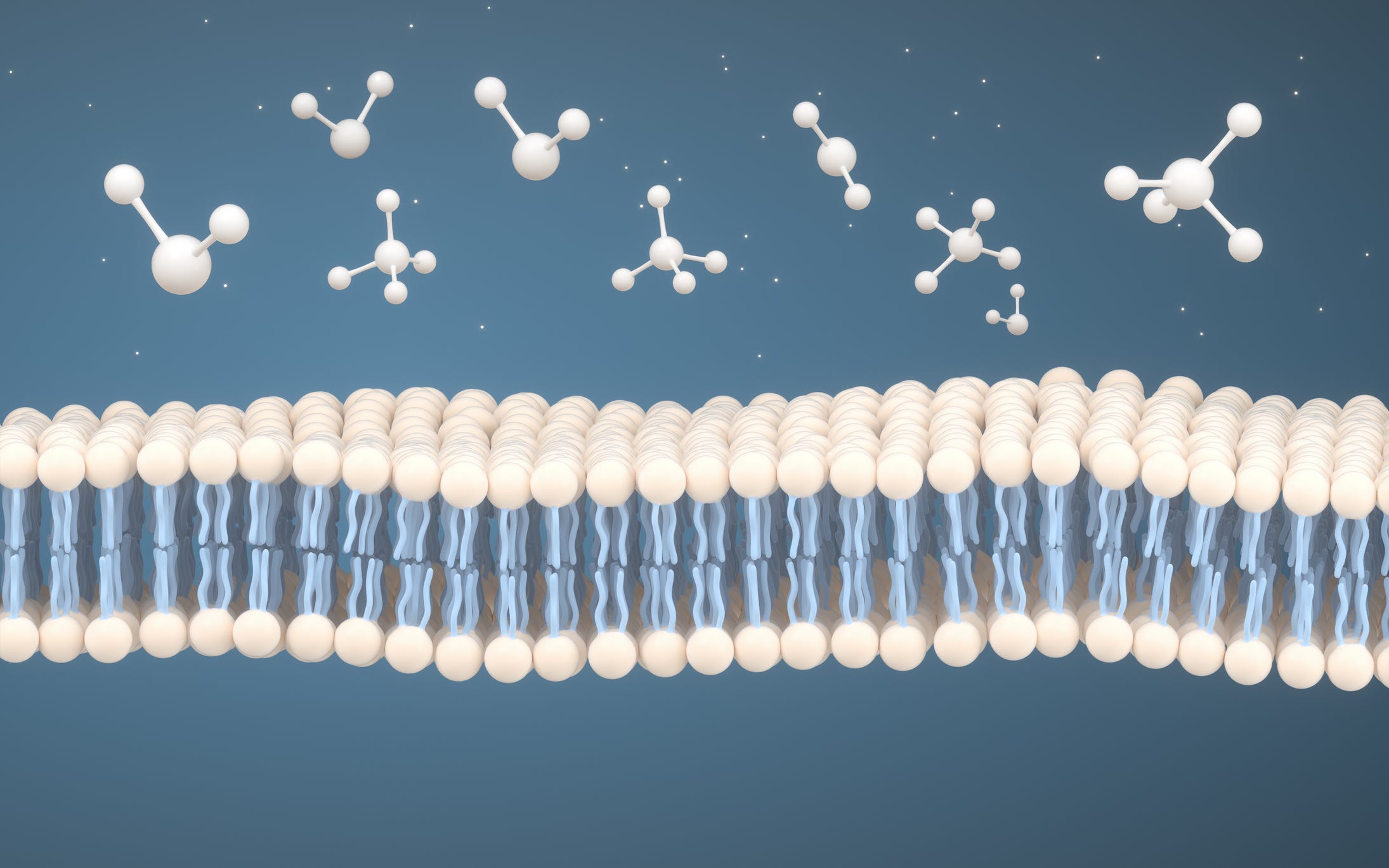
And we aren't just talking about women's fertility here. Low sperm count and other factors that contribute to male infertility are also on the rise. While age, genetics, and medical conditions play significant roles, environmental factors such as exposure to endocrine-disrupting chemicals (EDCs) are becoming recognized as contributors to fertility issues in both men and women.
Beyond hormonal disorders and genetic predispositions, exposure to EDCs from pesticide residues and microplastics can disrupt the delicate balance of the endocrine system, potentially impacting fertility in both men and women. Research suggests these chemicals may interfere with reproductive hormone function, leading to menstrual irregularities, decreased sperm quality, and difficulty conceiving.4
Having in-depth conversations with your patients and referring them to fertility specialists is vital to managing their health and well-being. It's important for couples trying to conceive to realize they are not alone.
Since women bear the brunt of the physical and emotional challenges of bringing life into this world, let's explore some common areas that may be signs of female infertility or potential risks for becoming pregnant.
7 Potential Signs of Infertility in Women
Atypical menstruation can affect a woman's ovulation. Anovulation is a condition where a woman who is of childbearing age does not have regular menstrual periods, thereby affecting her ability to become pregnant. Research indicates approximately 30% of infertility cases are due to anovulation.5
1. Ovulation Disorders
For many women, experiencing abnormal ovulation, irregular periods, or an absence of her period may be indicative signs of infertility. Ensuring that you are having conversations about the whole person and their health journey can help you to work closely with your patients to identify areas that may be affecting their fertility and overall health.
- Polycystic Ovarian Syndrome (PCOS)
Polycystic ovarian syndrome is a hormonal disorder that is considered a common sign of female infertility, affecting about 10% of women of childbearing age living in the U.S.6 This upheaval in a woman's hormonal balance is caused by an increase in the male hormone androgen, causing irregular or missed periods and cysts along the outside of the ovaries (polycystic), all affecting regular ovulation. These polycystic ovaries contain follicles or immature eggs that fail to be released normally.7 In some cases, a woman may also present with weight gain, pelvic pain, severe acne, male pattern baldness, and hair growth on the face and chest.
Additionally, women with PCOS may also produce too much insulin, causing metabolic concerns like insulin resistance, where the body is not able to use endogenous insulin effectively.8 If left unmanaged, it can result in issues with healthy glucose metabolism and other health concerns. - Primary Ovarian Insufficiency (POI)
Primary ovarian failure is a condition where a woman's ovaries stop working before age 40. It causes irregular menstrual periods and may be another sign that leads to infertility.9 POI is characterized by missed or irregular periods for four months after having had regular periods for a while. Follicle-stimulating hormone (FSH) levels are high, and estrogen levels are low.10
Wellness providers should also thoroughly investigate their patients' family history or genetics since this may be another cause of primary ovarian insufficiency, which a specialist must assess and manage.
2. Weight Concerns: Too Much and Too Little
When assessing their health behaviors, it is essential to discuss your patient’s dietary habits and physical activity level. Body mass may impact fertility, so women and men should strive to maintain a healthy body weight.
Women with a body mass index (BMI) greater than 27kg/m2 may experience anovulation. Obesity can cause a woman's body to produce too many androgens, impacting her ovaries' ability to produce mature follicles for regular ovulation.11 Women may improve ovulation by losing about 10% of their body weight.12
Some factors of obesity may influence the male reproductive system, including abnormally high insulin levels of endogenous insulin (hyperinsulinemia), leptin resistance, and oxidative stress. Obesity, therefore, can impact male fertility and the reproduction potential, including sperm concentration, motility, and viability.13
Also, women who have a BMI of less than 17kg/m2 and a lifestyle that includes extreme exercise regimens or have disordered eating habits often present with infertility due to irregular ovulation.12 The treatment plan can include correcting energy deficits and modifying lifestyle.
3. A Woman's Age
By age 30, a woman may experience a decline in her fertility. If your patient is age 35 or older and has not been able to conceive for six months or longer or is over the age of 40, referring to a fertility specialist may be the best next step.14
4. Fallopian Tube Issues
Fallopian tube blockages or fibroids that can obstruct the fallopian tubes can impact fertility. Other tubal dysfunction can result from pelvic inflammatory disease (PID), an ectopic pregnancy, or pelvic adhesions from lower abdominal surgery.15
5. Endometriosis
BPA (bis-phenol-A), a commonly used plasticizer and preservative in canned goods, fundamentally changes the neuroendocrine pathways involved in reproductive health and has been associated with fewer antral follicles and oocytes in women receiving fertility treatment and those diagnosed with endometriosis or PCOS.4 A lower number of antral follicles and oocytes can indicate potential issues with ovarian function, which may affect a woman's ability to conceive.
Endometriosis can also impair fertility secondary to causing tubal, uterine, or other lesions.15
6. Lifestyle Influences
Lifestyle factors, such as stress, excessive alcohol consumption, smoking, and sexually transmitted diseases, can adversely affect fertility. Excessive stress can cause an imbalance in critical hormones, which include gonadotropin-releasing hormone (GnRH), luteinizing hormone (LH), and follicle-stimulating hormone (FSH) that all play an integral role in regular ovulation.16
Discussing ways to manage stress and other factors that may improve your patients' physical and emotional well-being is vital in helping them achieve optimal health and support fertility.
7. Recognizing Environmental Factors Impacting Reproductive Health
Beyond hormonal disorders and genetic predispositions, exposure to EDCs from pesticide residues and microplastics can disrupt the delicate balance of the endocrine system, potentially impacting fertility in both men and women. Research suggests that these chemicals may interfere with reproductive hormone function, leading to menstrual irregularities, decreased sperm quality, polycystic ovarian syndrome, endometriosis, hormone-sensitive cancers, precocious or delayed puberty, difficulty conceiving, and adverse birth outcomes.4
Empowering Patients for Holistic Health
As wellness practitioners and patient advocates, identifying signs of infertility and having a candid conversation with your patients to help them understand and manage reproductive health challenges and medical conditions is essential.
Engaging in open dialogues with patients about the multifaceted nature of infertility is essential. Educating patients about the potential impact of environmental factors, such as pesticide residues and microplastics, empowers them to make informed choices to protect their reproductive health.
Key Considerations for Patients:
- Recognizing the inevitable connection between an individual's diet and fertility may empower them to make healthier choices in the short and long term. An in-depth dietary analysis and nutritional consultation help fully assess the patient's intake and identify nutritional gaps.
- Current studies indicate that a diet based on the Mediterranean Diet (MeD) recommendations can positively influence your patient's mental and physical health. Consuming a whole-food diet that limits processed foods and harmful pesticide residues has also been associated with favorable changes in insulin resistance and the risk of obesity, which is crucial for fertility.17
- Choose organic foods whenever possible to minimize exposure to pesticide residues.
- Opt for non-toxic household products and reduce plastic use to limit microplastic exposure.
By addressing environmental influences on fertility alongside traditional risk factors, healthcare providers can better support patients in their journey toward conception. Patients and wellness providers must advocate for policies that prioritize environmental health and regulate the use of EDCs to safeguard reproductive well-being for generations to come.
Together, we can navigate the complexities of infertility and empower individuals to prioritize their reproductive health in an increasingly chemical-laden world.
‡ The products and claims made about specific products on or through this Site have not been evaluated by the United States Food and Drug Administration and are not approved to diagnose, treat, cure, or prevent disease.
‡ This Site is not intended to provide diagnosis, treatment, or medical advice. Products, services, information, and other content provided on this Site, including information that may be provided on this Site directly or by linking to third-party websites are provided for informational purposes only. Please consult accredited healthcare professional organizations, evidence-based herbal monographs, and published clinical research regarding any medical or health-related diagnosis or treatment options.
References:
1. Cleveland Clinic. “Infertility.” 2023, Infertility: Types, Causes, Symptoms, Diagnosis & Treatment (clevelandclinic.org). Accessed 1 May 2024.
2. World Health Organization. “1 in 6 people globally affected by infertility: WHO.” 2023, 1 in 6 people globally affected by infertility: WHO. Accessed 1 May 2024.
3. Office on Women's Health. “InfertilityWomenshealth.gov.” 2018, Infertility | Office on Women's Health (womenshealth.gov). Accessed 1 May 2024.
4. Yilmaz B, Terekeci H, Sandal S, Kelestimur F. Endocrine disrupting chemicals: exposure, effects on human health, mechanism of action, models for testing and strategies for prevention. Rev Endocr Metab Disord. 2020;21(1):127-147. doi:10.1007/s11154-019-09521-z Accessed on 9 May 2024.
5. Skoracka, Kinga et al. “Female Fertility and the Nutritional Approach: The Most Essential Aspects.” Advances in nutrition (Bethesda, Md.) vol. 12,6 (2021): 2372-2386. doi:10.1093/advances/nmab068. Female Fertility and the Nutritional Approach: The Most Essential Aspects - PMC (nih.gov). Accessed 1 May 2024.
6. Cleveland Clinic. “Polycystic Ovary Syndrome (PCOS) & Treatment.” Cleveland Clinic, 21 Sept. 2021, my.clevelandclinic.org/health/diseases/8316-polycystic-ovary-syndrome-pcos. PCOS (Polycystic Ovary Syndrome): Symptoms & Treatment (clevelandclinic.org). Accessed 1 May 2024.
7. Mayo Clinic. “Polycystic Ovary Syndrome (PCOS) - Symptoms and Causes.” 2022. www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439. Accessed 1 May 2024.
8. www.eatright.org. “Polycystic Ovarian Syndrome.” 2023 www.eatright.org/health/pregnancy/fertility-and-reproduction/polycystic-ovarian-syndrome. Accessed 1 May 2024.
9. Cleveland Clinic. “Primary Ovarian Insufficiency.” 2022. Primary Ovarian Insufficiency: Causes, Symptoms & Treatment (clevelandclinic.org). Accessed 1 May 2024.
10. Eunice Kennedy Shriver National Institute of Child Health and Human Development - NICHD. “Primary Ovarian Insufficiency.” https://www.nichd.nih.gov/health/topics/factsheets/poi. Accessed 3 May 2024.
11. Cleveland Clinic. ”Anovulation.”https://my.clevelandclinic.org/health/diseases/21698-anovulation 2024, https://my.clevelandclinic.org/health/diseases/21698-anovulation. Accessed 1 May 2024.
12. Walker MH, Tobler KJ. Female Infertility. [Updated 2022 Dec 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556033/ . Accessed 3 May 2024.
13. Obradovic, Milan et al. “Leptin and Obesity: Role and Clinical Implication.” Frontiers in endocrinology vol. 12 585887. 18 May. 2021, doi:10.3389/fendo.2021.585887. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8167040/. Accessed 3 May 2024.
14. Mayo Clinic. “Infertility-Symptoms and Causes.” 2023, https://www.mayoclinic.org/diseases-conditions/infertility/symptoms-causes/syc-20354317. Accessed 3 May 2024.
15. “Tubal dysfunction and Pelvic Abnormalities - Gynecology and Obstetrics.” MSD Manual Professional Edition, www.msdmanuals.com/professional/gynecology-and-obstetrics/infertility-and-recurrent-pregnancy-loss/tubal-dysfunction-and-pelvic-abnormalities. Accessed 9 May 2024.
16. Rooney, Kristin L, and Alice D Domar. “The relationship between stress and infertility.” Dialogues in clinical neuroscience vol. 20,1 (2018): 41-47. doi:10.31887/DCNS.2018.20.1/klrooney. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6016043/ . Accessed 4 May 2024.
17. Skorack, Kinga, et al. “Female Fertility and the Nutritional Approach: The Most Essential Aspects.” Advances in nutrition (Bethesda, Md.) vol. 12,6 (2021): 2372-2386. doi:10.1093/advances/nmab068. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8634384/ . Accessed 4 May 2024.
Jenny Perez is an herbal educator, researcher, and writer who has been immersed in the field of nutrition and botanical medicine for more than 20 years. Jenny has created curriculum, content, and educational materials for Quantum Nutrition Labs, Premier Research Labs, the American Botanical Council, and Bastyr University’s Botanical Medicine Department where she was Adjunct Faculty, Herb Garden Manager, and Director of the Holistic Landscape Design certificate program.